NC Providers Council Legislative & Policy Initiatives
2023 LEGISLATIVE PRIORITIES
Working in tandem with the Providers Council Board and standing Committees comprised of Provider and Provider Support members, the lobbyists are ensuring that the Providers Council’s legislative priorities are communicated to key Committee Chairs and Members during the 2023 Long Session.
The NC Providers Council has a great reputation for its analysis of legislation, administrative rules, and Medicaid State Plan, waiver, and clinical coverage policy provisions impacting community services funded through the North Carolina General Assembly and North Carolina Department of Health and Human Services (DHHS). With our active involvement at the General Assembly through Maynard and Associates, collaboration with numerous Divisions of DHHS – including participation in statewide workgroups and Committees, and an ongoing, constructive dialogue with Standard Plan and LME/MCO leadership, the association advocates for providers and the people who we support.
Legislative Session bill trackers and other documents related to NC Providers Council legislative advocacy are posted on the password-protected Member Communications page.
2023 State Budget Update: Although the State Fiscal Year begins each July 1, the NC General Assembly has not yet enacted a new biennium State budget. House and Senate leaders have communicated that they do not anticipate a vote before late July. The NCGA authority for Medicaid Expansion in Session Law 2023 – 7 is contingent on the NCGA enacting a State budget.
Medicaid Expansion will begin the later date of:
Effective date of the State budget / Appropriations Act; OR
CMS approval of the NC Medicaid Expansion State Plan Amendment.
OLMSTEAD UPDATES
Olmstead v. L.C., 527 U.S. 581 (1999), is a U.S. Supreme Court case that laid the groundwork for people with disabilities to live their lives as fully included members of the community. The case addressed the Americans with Disabilities Act’s (ADA) “integration mandate.” The integration mandate requires that all public entities, including the State of North Carolina, “administer services, programs, and activities” for people with disabilities in the most integrated setting appropriate to the person’s needs. “Most integrated setting” has been defined as one that enables people with disabilities to interact “to the fullest extent possible” with individuals that don’t have a disability. Specifically, the case requires states to provide services in the community for eligible persons with a disability when (a) such services are appropriate; (b) the affected persons do not oppose community-based treatment; and (c) community-based services can be “reasonably accommodated.”
In December of 2021, the State Of North Carolina published its long-range plan for Olmstead compliance.
In addition to relevant legislation that has been filed during the 2023 Long Session, the North Carolina Providers Council is monitoring the NC Medicaid program’s regulatory and policy environment for any related changes that may arise. The Providers Council uses its bi-weekly member policy newsletter and standing Committee and workgroup meetings to keep members apprised of developments in these two lawsuits of interest. You can learn more about the benefits of an NC Providers Council membership here.
FEDERAL PUBLIC HEALTH EMERGENCY (PHE) SUNSETTED MAY 11, 2023
From January 2020 to January 2023, the U.S. Health and Human Services Secretary declared and extended the federal Public Health Emergency in 90-day increments. The Public Health Emergency ended on May 11, 2023. Many temporary policy flexibilities in Medicaid State Plan and Waiver programs and clinical coverage policies were linked to the federal Public Health Emergency. Those flexibilities are going to sunset in 2023. In addition to temporary policy flexibilities, a federally appropriated 6.2% enhanced Federal Medical Assistance Percentage (FMAP) or “match” for State dollars that North Carolina DHHS receives from the federal Centers for Medicare and Medicaid Services (CMS) for every dollar spent on Medicaid services is phasing out in 2023. The enhanced FMAP has enabled NC DHHS to temporarily increase health plan and provider reimbursement rates. Although the State Medicaid agency has requested 2023 State budget appropriations to help offset the loss of PHE-related enhanced rates, the NC General Assembly had not yet enacted a State budget by the July 1, 2023 beginning of the new State Fiscal Year. As a result, some PHE-related enhanced rates, including those for Personal Care Services within certain service settings, ended on June 30, 2023. The State Medicaid agency, the Division of Health Benefits, has reported the following: “Once a State budget has been finalized, NC Medicaid will implement any permanent increases at the levels appropriated in the budget and intends to systematically reprocess claims (or direct managed care organizations to reprocess claims, as applicable) retroactive to July 1 to adjust payments to the level of the appropriated permanent increases. This reprocessing will ensure that providers receive the full value of the legislated increases. For more information, please see SPECIAL BULLETIN COVID-19 #267: Temporary COVID-19 Rate Increases Ending June 30, 2023.”
The CMS schedule to phase out the enhanced match is:
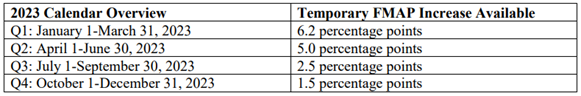
Source: SHO-23-002 (medicaid.gov)
Clinical Coverage Policy Flexibilities Sunsetting
In early 2020, the North Carolina Department of Health and Human Services (NC DHHS) received approval from the federal Centers for Medicare and Medicaid Services for several waivers under the COVID-19 Public Health Emergency. The waivers authorized temporary policy flexibilities for Medicaid State Plan and Waiver services and NC Health Choice services. Access all relevant NC DHHS documentation and summaries here.
NC Medicaid Special Bulletin COVID-19 #237, Extension of NC State of Emergency Temporary Flexibilities, outlined a Policy Flexibilities Sunsetting Schedule. It lists:
- Flexibilities that have been made permanent in clinical coverage policy;
- Flexibilities that ended on June 30, 2022; and
- Flexibilities that will end with the federal PHE or 6 months after the end of the PHE (November 11, 2023).
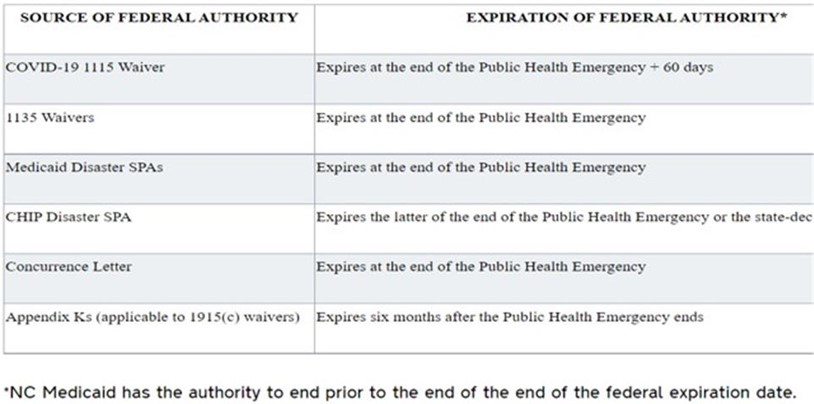
This NC DHHS summary table outlines the sunset timing for temporary policy flexibilities associated with specific COVID-19 NC DHHS waivers:
Medicaid Program Eligibility Redeterminations and Disenrollment Began April 1, 2023
Although the federal PHE ended on May 11, the Congressional Omnibus Budget Act signed into law in late 2022 authorized State Medicaid programs to begin disenrolling Medicaid beneficiaries who have remained enrolled during the PHE regardless of their eligibility status beginning April 1, 2023. As a condition of receiving the aforementioned 6.2% enhanced FMAP, State Medicaid programs have been prohibited from terminating individuals’ Medicaid program enrollment during the PHE. An estimated 400,000 or more individuals may be deemed ineligible for the program and disenrolled beginning July 1, 2023, as the state’s County DSS offices process the redeterminations during a 12-month period. Some individuals who lose their Medicaid enrollment will qualify for health insurance on North Carolina’s Federally Facilitated Exchange or “Marketplace” at https://www.healthcare.gov. For individuals who lose their Medicaid enrollment for administrative reasons (failure to return a renewal form or other necessary information timely), CMS has authorized States to reconsider eligibility without requiring a new application if individuals submit the necessary information within 90 days of eligibility termination.
Because each State Medicaid program will be completing these critical eligibility redeterminations, the Federal Communications Commission published relevant Guidelines at the request of U.S. HHS Secretary Xavier Becerra to authorize State Medicaid programs to use text messaging, pre-recorded calls, and auto-dialed calls to contact individuals regarding Medicaid program eligibility and enrollment requirements. These would typically violate FCC robocall and robotext prohibitions [Source: FCC Provides Guidance to Enable Critical Health Care Calls | Federal Communications Commission]. The goal is to facilitate the redetermination process due to the high volume of individuals to be contacted, and to prevent any lapse in health insurance coverage for the individuals affected.
You can access detailed information regarding the NC DHHS “PHE Unwinding” process via the two State resources below:
- NC PHE Unwinding Plan as submitted to CMS: State Report on Plans for Prioritizing and Distributing Renewals (ncdhhs.gov)
- NC DHHS PHE Unwinding Dashboard and federally mandated reports: Federally Required Reports | NC Medicaid (ncdhhs.gov)
2023 LEGISLATIVE SESSION ISSUE WATCH: MEDICAID EXPANSION
History of Medicaid Expansion Legislation in NC
In 2010, Congress enacted the Affordable Care Act which included a mandate for States to expand their Medicaid programs.
In 2012, the U.S. Supreme Court heard a case regarding whether the federal government had overreached its authority, and the Opinion gave discretion to State governments regarding whether to expand Medicaid enrollment. North Carolina was one State that did not pursue Medicaid expansion. There are 11 non-expansion States remaining today. Initial arguments in the North Carolina General Assembly were that the federal government would not continue the high 90% Federal Medical Assistance Percentage match in the long run for the additional program beneficiaries enrolled, and that the State would ultimately bear a financial burden for the State dollars needed to make up for the regular Federal Medical Percentage match that is lower.
In 2013, the North Carolina General Assembly enacted law to preclude any NC Department of Health and Human Services pursuit of a State Plan Amendment for Medicaid expansion approval with the Centers for Medicare and Medicaid Services [S.L. 2013-5, Section 3]:
Since 2017 [See HB662 “Carolina Cares” bill], any time an NCGA Member has filed a bill for some form of Medicaid expansion, the bill has contained two additional, politically contentious provisions in some form:
-
- Work requirements for individuals who would be eligible to enroll; and
- Assessments on health care system providers including hospitals and health plans to fund the 10% State match to the 90% Federal Medical Assistance Percentage so the expansion would not require any additional State appropriations.
From 2017 – 2021, the Trump administration approved Medicaid expansion State Plan Amendments with work requirements. However, beginning in 2022, the Biden administration retracted those approvals and it is currently not possible to get Centers for Medicare and Medicaid Services approval for a Medicaid expansion plan that includes a work requirement.
2022 Legislative Activity and Negotiations
During the 2021 legislative session, the General Assembly enacted law [S.L. 2021-180, Section 5.13] to require the convening of a bicameral Joint Legislative Committee on Access to Healthcare and Medicaid Expansion “. . .to consider various ways in which access to health care and health insurance can be improved for North Carolinians, including those individuals described in section 1902(a)(10)(A)(i)(VIII) of the Social Security Act.” [individuals < 65 years of age; not pregnant; living with a household income < 133% of the Federal Poverty Level; and not entitled to or enrolled in Medicare]. The Committee met throughout the spring of 2022. Presentations included speakers who supported and opposed Medicaid expansion and separate regulatory and scope of practice issues being considered in tandem to increase access to care if Medicaid expansion were to be implemented in the State.
In 2022, we saw Medicaid expansion bills filed in the House and Senate:
- HB149: Expanding Access to Healthcare
- Medicaid Expansion with hospital assessments to cover the 10% State match
- Increased hospital reimbursement
- Work requirements (if federally approved)
- Expanded scope of practice for Advance Practice RNs
- Certificate of Need Regulatory Reform
- SB408: Rural Healthcare Access & Savings Plan Act
- Medicaid Expansion with hospital assessments to cover the 10% State match
- American Rescue Plan Act funding for Opioid treatment
- Rural healthcare access plan
- Work requirements (if federally approved)
House Bill 149 was worked in both Chambers. The primary reasons for the bill not passing were:
- Certificate of Need regulatory reform impasse;
- Advance Practice Registered Nurse expanded scope of practice reform impasse; and
- Some Members were fundamentally opposed to Medicaid expansion.
2023 Session Bill Activity
The first year of a new State budget biennium – a “long session” year in North Carolina – convened on January 11th. The North Carolina’s General Assembly House and Senate seat composition has changed significantly in terms of the number of new Members and one Democrat changing party affiliation to Republican in April of 2023, so there is a Republican supermajority (enough votes for veto overrides) with a Democratic Governor. The NC DHHS Secretary and the Governor have implored the NCGA to enact Medicaid expansion for numerous years. This year, the State would receive a $1.8 billion bonus payment for becoming an expansion state and a 5% enhanced Federal Medical Assistance Percentage match for two years for the non-expansion Medicaid beneficiaries (there are currently 2.9M beneficiaries in NC) as authorized in the American Rescue Plan Act of 2021. The current enhanced match for non-expansion Medicaid beneficiaries is 73.91 cents of federal funding per dollar spent.
On February 8, 2023, the NCGA House of Representatives filed a Medicaid expansion bill (HB76, Access to Healthcare Options). On March 2, 2023, House and Senate leadership held a press conference to announce that they had reached an agreement to enact Medicaid expansion legislation. On March 27th, Governor Cooper signed the bill into law. It is now codified as Session Law 2023 – 7.
Although HB76 became law on March 27th, Medicaid Expansion will not begin immediately.
a. However, staggered implementation of the Certificate of Need exemptions will begin in the following order:
i. Immediately: psychiatric beds and facilities; chemical dependency treatment beds and facilities; replacement equipment up to $3 million, indexed to inflation; aggregate total of $3 million for all the equipment at a diagnostic center that individually exceeds $10,000; and Early and Periodic Screening, Diagnosis, and Treatment services to children under age 21 at home health agencies in compliance with federal law.
ii. Two years after first HASP payment: ambulatory surgical centers that commit 4% of earned revenue to charity care and operate in counties with >125K population.
iii. Three years after first HASP payment: MRI machines in counties with >125K population.
The NCGA authority for Medicaid Expansion in Session Law 2023 – 7 is contingent on the NCGA enacting a State budget. Medicaid Expansion will begin the later date of:
b. Effective date of the State budget / Appropriations Act; OR
c. CMS approval of the NC Medicaid Expansion State Plan Amendment.
The North Carolina Providers Council is monitoring the NC Medicaid program’s regulatory and policy environment as filed House and Senate bills continue to move through NCGA Committees and Chambers. The Providers Council uses its bi-weekly member policy newsletter and standing Committee and workgroup meetings to keep members apprised of developments when new laws are enacted. You can learn more about the benefits of an NC Providers Council membership here.
QUALIFIED PROFESSIONAL EDUCATION WAIVER HISTORY AND STATUS
- In 2013, the General Assembly enacted N.C.G.S. 108A-54.1B. to give DHHS State Plans and Waivers the force and effect of rules. Part (d) of that statute reads, “State Plans, State Plan Amendments, and Waivers approved by the Centers for Medicare and Medicaid Services (CMS) for the North Carolina Medicaid Program and the NC Health Choice program shall have the force and effect of rules adopted pursuant to Article 2A of Chapter 150B of the General Statutes.”
- In 2017, Session Law authorized an expansion of Qualified Professional hiring qualifications to include pre-education work experience in addition to post-education work experience.
- In 2018, the Centers for Medicare and Medicaid Services (CMS) approved this North Carolina Medicaid program State Plan Amendment to “allow all years of both pre-graduation and post-graduation full-time MH/DD/SAS experience to apply to the qualifications required for MH/DD/SAS Qualified Professionals.” The 2018 State Plan Amendment has the force and effect of rule [“NC Administrative Code”].
- In 2019, DMH/DD/SAS promulgated temporary administrative rule amendments to 10A NCAC 27G .0104 and 10A NCAC 28A .0102 to reflect the 2017 Session Law. However, the temporary rule amendments expired within six months. The content linked here is for historical reference only. If you open the two rules today, they will be in their original form and will not reflect the 2017 Session Law. However, because the 2018 State Plan Amendment has the force and effect of rule, the hiring practice of applying both pre- and post-education experience for Qualified Professionals is still authorized.
- In 2020, DMH/DD/SAS obtained Commission on DMH/DD/SAS approval for a “rule waiver” since the temporary rule amendments had expired. The rule waiver expired on 12/31/2021.
- In 2022, DMH/DD/SAS obtained approval for a new rule waiver request. The renewed rule waiver will expire in 12/2023. The rule waiver gives DMH/DD/SAS until December of 2023 to complete the permanent (versus temporary or emergency) rulemaking process so the administrative rules can finally reflect the QP qualification changes authorized in the 2017 Session Law and in the 2018 Medicaid program State Plan Amendment.
- In 2023, DMH/DD/SUS posted the proposed permanent rule amendments for Subchapters 10A NCAC 27G .0104 and 10A NCAC 28A .0102 for a 60-day public notice and comment period that ended on September 1, 2023. The rules were presented for approval at the November 2023 meeting of the Commission on DMH/DD/SUS. The rules were then presented for approval at the December 2023 meeting of the Rules Review Commission in the Office of Administrative Hearings. The rules were approved with an effective date of January 1, 2024.
NORTH CAROLINA GENERAL ASSEMBLY QUICK LINKS
- Click here to access NCGA Session Laws enacted during the 2023 long session.
- North Carolina General Assembly Home Page with Daily House and Senate Calendars for the 2023 Long Session http://www.ncleg.net/
- You can “find your legislators” by District or County by simply entering your mailing address into the prompt on this NCGA Web page: Representation – North Carolina General Assembly (ncleg.gov)
- NCGA Member Directory
- NCGA Committees https://www.ncleg.gov/Committees
- Fiscal Research Division https://www.ncleg.gov/FiscalResearch/
- Program Evaluation Division https://www.ncleg.gov/PED/
2023 NC PROVIDERS COUNCIL STATEWIDE COMMITTEE AND WORKGROUP PARTICIPATION
- Mental Health Coalition
- Developmental Disabilities Consortium
- Substance Use Disorder Federation
- The Coalition
- Provider-LME/MCO Leadership Forum
- DHB – DMH/DD/SAS – Provider Forum
- *Some members also serve on LME/MCO Provider Councils and Boards